Periods can be stressful: they’re associated with pain and obviously there’s all the products that go with them, like tampons and pads (and pain meds). So there’s more than enough reason to feel worried when you’re confronted with breakthrough bleeding or spotting right in the middle of your cycle. Luckily, there’s mostly nothing much to worry about.
What is breakthrough bleeding?
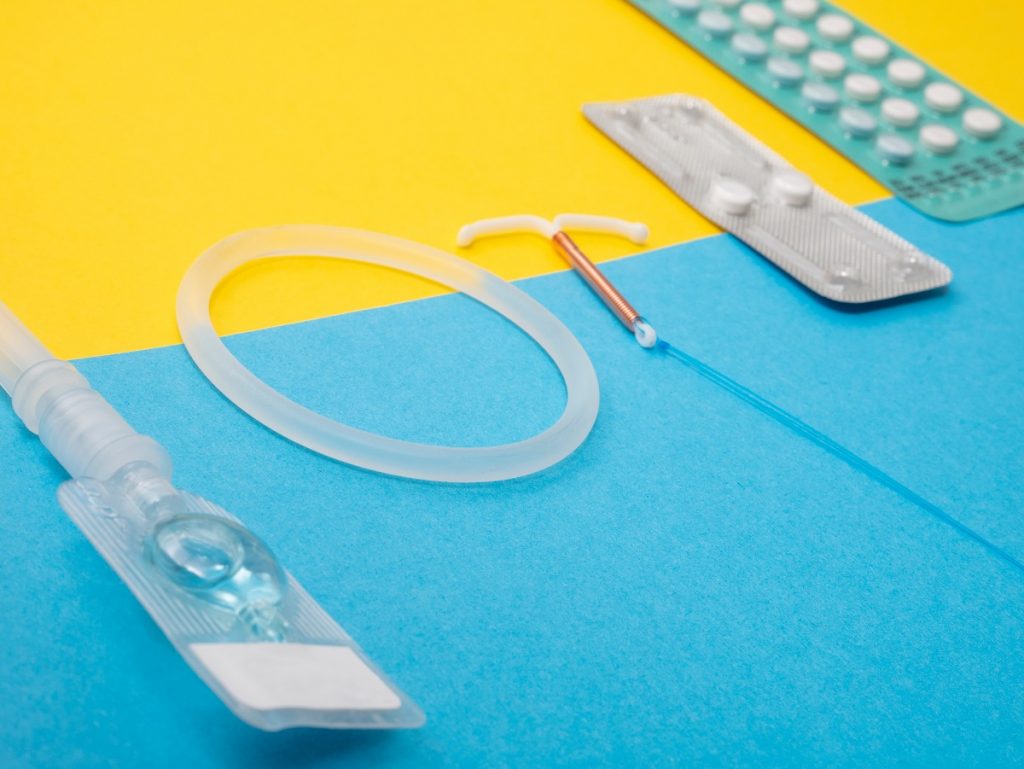
Breakthrough bleeding, also called spotting, occurs in the middle of the cycle or at any time when your regular period isn’t meant to be. They’re mostly associated with women on contraceptives. It’s estimated that 20% of contraception users experience irregular bleeding at some point, but it usually settles after a while.
Breakthrough bleeding is thought to be hormonal, but there isn’t much known about its origins.
Spotting is not a normal period and it’s also not the bleeding that happens when you’re on contraception – that’s called a withdrawal bleed, and happens when you take the placebo pills in your oral contraception or take out your vaginal ring for a few days to allow bleeding to occur. If you’re on the patch, your withdrawal bleeding will happen when you take off the patch for a week.
When does breakthrough bleeding occur?
Breakthrough bleeding mostly occurs when you switch to birth control, and is associated with your body’s adjustment to new hormonal levels that contraception releases. It should last a few days per cycle and stop after three to four months, when the body has gotten used to the birth control regimen.
Spotting can also happen if you’re not taking your birth control properly: every day at the same time. Skipping days can throw the hormonal balance out of whack, leading to breakthrough bleeding.
In one study, researchers had women take the pill consecutively with no break, while another group took three days off. The research showed that allowing your body three days off contraception can minimise the occurrence of breakthrough bleeding, whereas the group who took contraception without breaks experienced more spotting.
When is breakthrough bleeding problematic?
Per the Journal of Family Practice, if spotting goes beyond four menstrual cycles, you should consider switching contraceptives to one with a higher oestrogen-to-progestin ratio.
There are also other underlying issues that could be at play, like smoking, interactions with other medications, pregnancy or inflammation of the cervix. If you suspect any of these, you should see a doctor (you can also consult with a doctor virtually via the Zoie app).
What should you do if you have spotting?
If spotting spans over more than four menstrual cycles, it’s time to chat to a doc. There could be an underlying condition at play, like fibroids, or an infection, like chlamydia or gonorrhoea.
However, if you’ve just started a new birth control, or haven’t been taking your contraception as you ideally should, this could lead to breakthrough bleeding. Studies also show that using the vaginal ring can reduce spotting in users.
If you’re still on your chosen contraception method, experts advise that you continue taking your contraception as directed, track your breakthrough bleeds using an app or calendar, and consider taking a three-day break from contraception, then go back on for at least a full 21 days. This helps shed the lining built up over a few months of continuous birth control use.
If you smoke, you’re more likely to experience breakthrough bleeding. You might want to think about quitting as one of your options.