If you’re a person with ovaries, chances are you’ve been on birth control. Many, many women start birth control when they first start their periods and stay with it for many years. But at some point, you may start thinking, “What would it be like without contraception?” For some, it could be a scary thought. Knowing as much as you can before making your decision can help you be prepared for what comes after going off birth control.
First, What Is Birth Control?
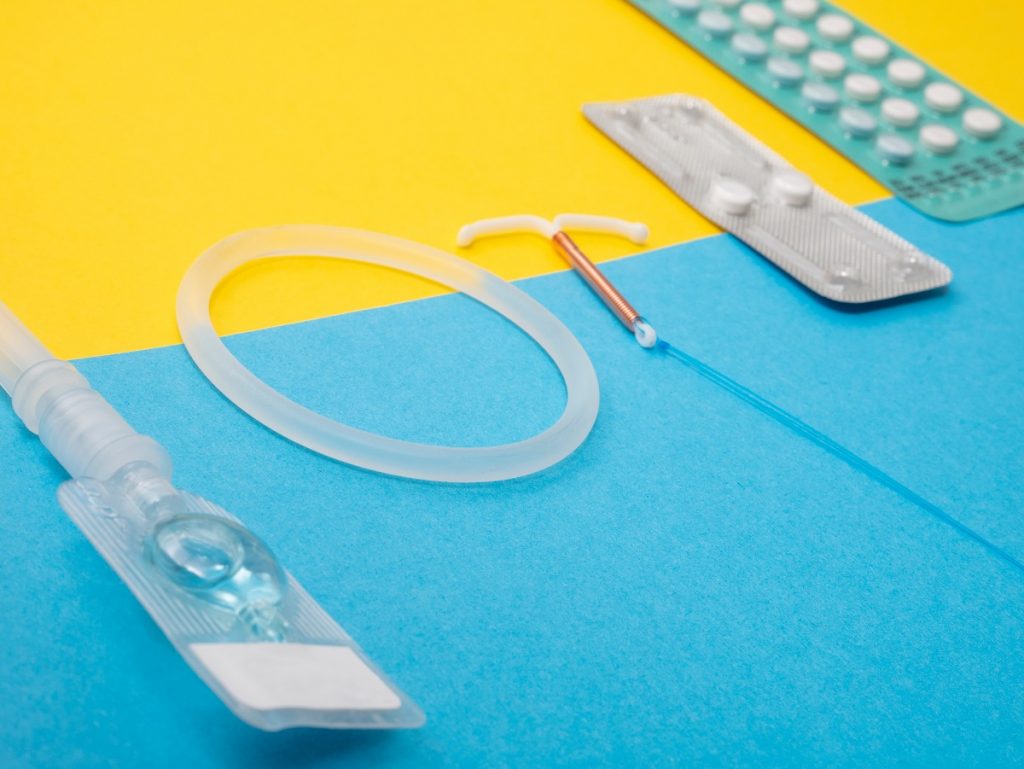
Birth control (BC), or contraception, are made up of synthetic hormones that create a hostile environment for sperm to thrive. Some halt ovulation completely, while others thicken cervical mucous, making it hard for sperm to reach and fertilise an egg. To be clear, we’re not referring to spermicides or barrier contraception methods, like condoms.
Because pharmaceutical contraception is made up of synthetic hormones, they work to regulate your natural hormonal production, which can impact your skin, weight, mood and of course, your menstrual cycle.
How To Go Off Birth Control
There’s no hard and fast rule for how to come off contraception. You could stop taking the Pill in the middle of your pack, remove your contraceptive ring, or have your IUD or implant removed. For injections, you could simply not go back for the next appointment and allow the hormones to leave your body.
If you’re not wanting to get pregnant, make sure that you use alternative contraceptives while you’re stopping contraception. You could use a barrier method like condoms or the diaphragm.
If you went on BC to treat an underlying condition, make sure you consult your doctor about stopping contraception to talk about how best to treat your condition. “Contraception unfortunately is usually used as a band-aid but doesn’t always solve the problem,” says Dr Ayo Oduntan, Zoie health educator and medical practitioner.
What Happens When I’m Going Off Birth Control?
When you’re going off birth control, you’re allowing the synthetic hormones progestin and estrogen (versions of the naturally-forming progesterone and oestrogen) to leave your body. These shifts cause changes in the body.
At first, you could experience a “breakthrough bleed”, which occurs when birth control is halted. The withdrawal from the medication is what typically happens when you take the placebo pills in your pack and experience monthly bleeding, in place of your natural periods.
Thereafter, your body will start reverting to its cycle pre-BC, whatever that looked like for you. You may experience the pre-menstrual symptoms more intensely, like:
- Pre-menstrual cramps
- Breast tenderness
- Bloating
- Moodiness
Your natural hormones could also create other symptoms, like:
- Acne
- More painful periods
- Changes in hair texture
- An increased libido
- Heavier or lighter periods than normal
How Long Does It Take For Contraception To Leave Your Body?
Synthetic hormones in your body only stick around for 48 hours, so you shouldn’t experience long-lasting effects after 90 days. These adjustments and a return to “normal” should happen in 90 days, according to experts.
Depo-Provera is linked to weight gain since it causes an increased appetite, so you might feel weight loss as a result of coming off the shot. It’s also the only birth control linked to a delay in ovulation when you’re off it – this could be as long as two years. For other birth control, you could be pregnant again in a year or less.
What If I’m Still Experiencing Something Off?
If you’re experiencing other effects, this might be a result of other things that your birth control was likely treating, like PCOS. Some symptoms that something else is at play could be abnormal uterine bleeding, period cramps and irregular cycles.
Contraception is usually prescribed when a patient is dealing with PCOS, fibroids, endometriosis, some cancers, and underlying bleeding conditions, but they’re for symptomatic management, says Dr Ayo. If you’re experiencing problems that are impacting your everyday life since coming off birth control, make an appointment with your doctor to ID what’s really at play.
Sources: Modern Fertility, PubMed, PubMed